Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Effectiveness of Educational Program on Incidence of Urinary Tract Infection and Vesico-ureteric Reflux among Non-Compliant Mothers of Spina Bifida Children at Cheshire Home, Khartoum State, Sudan
*Corresponding author: Ibrahim Ismail Mohammed Abu, Department of community medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia, Department of community medicine, Faculty of Medicine, Al Fashir University, North Darfur state, Sudan.
Received: December 05, 2024; Published: December 20, 2024
DOI: 10.34297/AJBSR.2024.25.003308
Abstract
Background: Clean Intermittent Catheterization was effective and safe in managing spina bifida patients with neurogenic bladder, its effectiveness needs compliance which is not previously documented in Sudan. The aim is to assess the effectiveness of educational program on frequency of urinary tract infection and vesico-ureteric reflux among non-compliant mothers of spina bifida children.
Subjects and Methods: quasi-experimental study design, which involves one group pre and post intervention. The study included 36 mothers of spina bifida children who weren’t compliant with clean intermittent catheterization at Cheshire Home. This educational program involved 36 non - compliant mothers 24(66.7%) mothers involved from December 2018 to December 2019, and it consisted of three phases. Phase 1. a) Pre intervention investigation of children with spina bifida (urine analysis and Micturating cysto-urethrogram (MCUG) b) all mothers filling the questionnaires which included their compliance about Clean Intermittent Catheterization. Phase2. An educational program which included a) Theoretical education about CIC b) Hands on practice of CIC c) Follow up for the first three months with urine analysis and voiding diary every month. Phase 3. After intervention with six months a) urine analysis, voiding diary and repeating the MCUG for those who had reflux. b) reviewing of the (compliance).
Results: the compliance changed significantly from pre to post at P value <0.05. There was no increase frequency of UTI. The VUR increased in post program in two patients out of seven (28.6%) and 5 (71.4%) showed improvement in VUR. Conclusion: The Education program showed effectiveness on improvement in renal function.
Keywords: Clean intermittent catheterization, Spina bifida, Vesico-ureteric reflux
Introduction
Spina bifida is a congenital neural tube defect which occurs either separately or in conjunction with hydrocephalus [1]. It develops in the early stage of pregnancy when one or more vertebrae fail to close normally. There are many types of spina bifida (SB) (spina bifida occulta, meningocele (MC), meningomyelocele (MMC)). Worldwide, the incidence of neural tube defects ranges from1.0 to 10.0 per 1000 births with almost equal frequencies between anencephaly and spina bifida [2]. In the United States, 1500 children are born with spina bifida every year [3]. In Africa, little is known about the incidence of MMC and neural tube defects. The incidence of SB and NTD in Nigeria and south Africa is.46/1000 births, while the incidence in Cameron was 1.99/1000 births [4]. In Sudan, the incidence of Neural Tube Defect in Omdurman Maternity Hospital 3.48/1000 births [5]. In other study the prevalence of neural tube defects in newborn admitted to neonatal intensive care unit in Soba University Hospital and Omdurman Maternity Hospital is 2.8/1000 births [6].
Children with spina bifida face many medical problems that challenge surgeons and pediatricians. The severity of the problems depends on the site of defect; one of these problems is neurogenic bladder and bowel dysfunction that occurs due to damage of the nerves that control bowel and bladder. Children with spina bifida have incontinence of stool and urine, which affects the quality of life, and75% of (SB) regard urinary incontinence as a stress factor [7].
Moreover, in children with spina bifida, renal failure maybe a long-term complication and it remain a major cause of death before adulthood due to damage of the kidney as a result of back flow of urine (Vesico-Ureteric Reflux) (VUR) [8].
Clean Intermittent Catheterization is defined by International Continence Society as the use of clean technique to drain the bladder with subsequent removal of catheter [9,10]. It could be done by patients, caregivers or parents. CIC was first introduced by Lapides, et al. in 1972 and they found that this technique is safe and effective in managing patients with neuropathic or atonic bladder if performed properly on regular intervals [9] Kaplan and Ellen, et al., reported that through CIC and medication, 85% of patients were able to stay dry for three to four hours [11].
Clean intermittent catheterization needs compliance and adherence to prevent urinary tract deterioration, World Health Organization (WHO) defines adherence as the extent of which persons behaviors corresponds with agreed recommendations from health care profession [12]. Compliance of patients with chronic diseases is very important for the success of management. Therefore, those who do not adhere or adhere partially develop major medical problems. Pohl, et al., described that early dropout from CIC among children and adolescents was 20%, so, good support, professional instruction on catheterization technique and periodic follow-up are necessary to maintain patient compliance [13].
Few studies explored the factors of non-adherence to CIC. Jai H. Seth, et al., mentioned that the barriers to successful CIC are internal factors which consist of patient-related factors that include the physical factor (practical), and the psychological factor (psychosocial and cultural aspects) which restrict its use. External factors involve the quality of teaching, supervision, follow-up and catheter availability in the community [9]. A study carried out in Saudi Arabia showed that the success rate of CIC among pediatric patients with neurogenic bladder resulting from MMC ranges from 94% to100% and that Saudi patients have good acceptance and compliance with CIC procedure and the researcher suggests that for complete success, proper education ,teaching and follow-up should be conducted [14].
Moreover SI Afsar, et al., evaluated the compliance with bladder emptying method at a long-term period among spinal cord injured patients and found that education of patients about catheterization technique and periodic follow-up are necessary to maintain patient compliance [15].
Hypotheses
H1: Sufficient information and thorough education will improve the practice related to clean intermittent catheterization and will decrease UTI and VUR which influences compliance and quality of life.
H0: Sufficient information and thorough education will not improve the practice related to clean intermittent catheterization and will decrease UTI and VUR, which influences compliance and quality of life.
Objective
1. To study mothers’ compliance regarding CIC pre- and post - program.
2. To estimate the frequency of UTI pre- and post- educational program.
3. To determine the incidence and grade of VUR pre- and postprogram and study the association between type of bladder and VUR.
4. To asses mothers’ compliance pre- and post-program.
5. To identify the relationship between compliance and some factors affecting compliance.
Materials and Methods
Its quasi-experimental study design, which involves one group pre and post test. The study was conducted in Khartoum Cheshire Home, which is located in Ebeid Khatim Street, Altaif, Khartoum. The home was founded in 1973 following an initiative of some Sudanese community leaders and the British ambassador to help disabled children similar to British Cheshire Home. The head of the executive committee is traditionally the British Ambassador in Khartoum.
The study started in December 2018. Pre- program investigation took two months then the program started in February 2019 to December 2019 It consisted of mothers of children with spina bifida who are not complying to CIC. Inclusion criteria: Mothers of children with spina bifida who received the training program but were not compliant for more than three months and Exclusion criteria New cases in CIC program.
According to relevant literature, the researcher used three tools:
First tool; A structured questionnaire which includes two parts:
Part 1;
A. Demographic data about children with spina bifida and their mothers which include child age, residence, father and mother occupation, marital status of parents, education level of parents, number of children and income.
B. Baseline medical information regarding spina bifida which includes type, site, associated with hydrocephalus, lower limb problem, operation and age of operation.
C. Baseline specific information regarding CIC that includes urethral sphincter control, age of the child when he or she started CIC etc.
Second tool; Compliance and satisfaction assessed by:
1. Compliance and satisfaction questionnaire including 12 close-ended Yes/No questions and one open-ended question categorized according to answers and responses. the pre means of Compliance was compared with the post means of compliance (P value< 0,05 is significant)
2. Voiding diary every month in the first three months, and post the program, those who have voiding diary according to prescribed schedule are considered compliant.
Statistical Analyses
All questionnaires were checked for completeness in the field. Data were coded, entered into a predesigned data sheet in a computer, cleaned and checked for inconsistencies using SPSS software version twenty.
The data were organized, tabulated and analyzed using Descriptive statistics in qualitative data while percentages, X2 and standard deviation were used in quantitative data.
Inferential statistics
T-tests were used to test if there is any significant difference between the pre-test and post-test proportions in pra compliance. This will be set at α (level of significance) 0.05% and 95% confidence level.
Fisher’s exact and Chi-squared tests were used for Association of compliance with three-month follow-up and post program, association between VUR, VUR site and VUR grade pre and post, and association between compliance and lower limb problems, number of children and child order.
Correlation and association between demographic data and practice and compliance used Spearman’s correlation coefficient.
Ethical Approvals
Written letter of permission was obtained from the Faculty of Nursing Sciences to the manager of Cheshire Home to apply for the educational program. Also, informed verbal consent obtained from mothers of children with spina bifida. Any mother can withdraw from the program at any time so that it does not affect her childcare.
Work Plan
Phase 1: assessment phase
1. Pilot study was carried out in 10% of the total sample twice (test and retest). The time required for filling the three tools was seven minutes. The tools were valid and reliable 0.973 and 0.986 sequences.
2. A. Frequency of UTI by doing urine specimen analysis, Micturating- cysto- urethrogram to assess the degree of vesico -ureteric reflux and urinary diary to assess the types of bladder and compliance B. Assessment compliance using a structured- interview questionnaire.
Phase 2: Implementing CIC educational program
Implementation of educational program of CIC phase 1. Training workshop is done in two forms:
Theoretical form of lecture (PowerPoint presentation), educational kits which include a book translated into simple Arabic, posters and brochure.
Phase 3: evaluation phase
Stage 1: The mothers were given appointments to see them after one week with urine diary for 48hours prior to consultation to examine adherence and evaluate the type of bladder so as to add oxybutynin intravesical if it is hyperactive. Then every one month with urine analysis and voiding diary for the 1st three months.
Stage 2: A. Filling the same questionnaires after three months. B. Post intervention Investigations; (MCUG. Urine specimen analysis) and voiding diary).
Statistical Analyses
A. All questionnaires were checked for completeness in the field. Data were coded, entered into a predesigned data sheet in a computer, cleaned and checked for inconsistencies using SPSS software version twenty.
B. The data were organized, tabulated and analyzed using Descriptive statistics in qualitative data while percentages, X2 and standard deviation were used in quantitative data.
C. Inferential statistics
1. T-tests were used to test if there is any significant difference between the pre-test and post-test proportions in compliance. This will be set at α (level of significance) 0.05% and 95% confidence level.
2. Fisher’s exact and Chi-squared tests were used for Association of compliance with three-month follow-up and post program, association between VUR, VUR site and VUR grade pre and post, and association between compliance and lower limb problems, number of children and child order.
3. Correlation and association between demographic data and compliance used Spearman’s correlation coefficient.
Results
A total of 36 noncompliant mothers of spina bifida children were approached, 24 mothers responded (response rate=66%). One (2,7%) child with bilateral VUR was excluded from the study due to Mitrofanoff operation Data were collected, analyzed statistically and the results were explained in figures and table.
54.2% of children under study were practicing CIC while 45.8% were not on CIC. 62.5% of children started CIC between the ages of 1-3years, while 25% started it from 4-7years, 4.2% were less than 1year and 8.3% started from 8-11 years as shown in Figure 1 below; (Figures 1,2 & Tables 1)
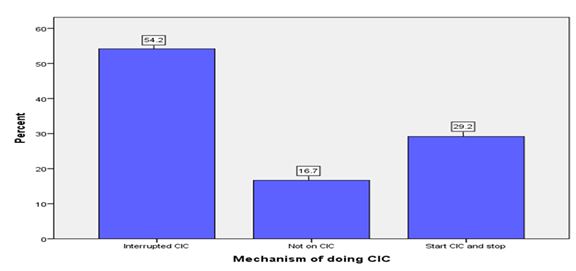
Figure 2: Mechanism of doing CIC in children under study(CIC= Clean Intermittent Catheterization)
As shown in Figure 2, 54.2% of children were on interrupted CIC while 29.2% started and stopped and 16.7% were not on CIC.
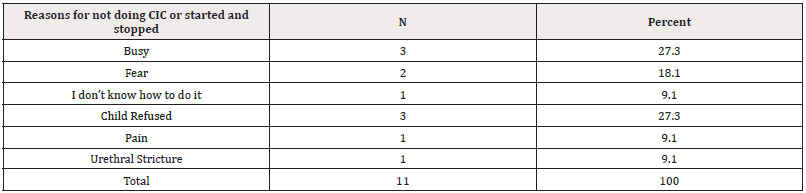
Table 1: Reasons for not doing CIC or started and stopped among study children.
Note*: CIC= Clean Intermittent Catheterization.
Regarding the association between satisfaction of participants pre and post the program. The P - value is significant as shown in Table 2.
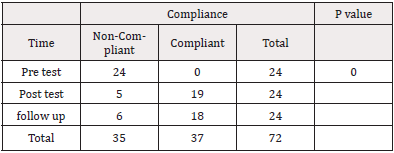
Table 3: Association of compliance with time (A three-month follow- up and post program) according to voiding diary.
Association of compliance during a three-month follow-up and post program, which was significant as shown in Table 3.
Frequency of UTI pre, a three-month follow-up and post program among study group which showed there is no increase frequency of UTI as in Table 4.
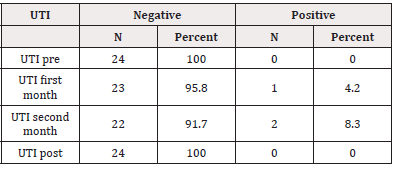
Table 4: Frequency of UTI pre, three months follow up and post program.
Note*: UTI= Urinary Tract Infection.
Seventy percent (70%) of study group had no VUR in MCUG while 30% had VUR preprogram as shown in Table 5.
Discussion
In this study the majority of patients were aged from 7 to 12yrs, this is the same with studies reviewed in which the ages of children above 15years is in one study and from 7 to 12 years is in another.
The majority of the mothers were housewives, most of the parents’ educational levels were high school and their incomes ranged from 3000-6000 SDG. Most of them had 4 to 6 children and the affected child was the third one. In this study, there was no association between the age of the child, number of children in the family, and educational level of parents and adherence. This is similar to the study reviewed, which examined the factors affecting adherence and found that only the income affects the adherence rate [16].
The majority of children started CIC early in their life from 1 to 3 years. Despite teaching the majority of mothers (75%) CIC verbally and through demonstration, the majority of them performed CIC but not at regular intervals, while others do not performed CIC at all. In our study, the barriers of irregular performance of CIC or not performing CIC were ignorance about the frequency in the majority. Other barriers include child going to school, mothers believing that the catheter causes UTI, some doctors advising their patients to perform CIC in three times interval /day, busy mothers and child refusing CIC, fear, pain and urethral stricture. One of these barriers is the same in the study reviewed in which it was found that CIC was done in non-school hours and preferred diapers during school hours [17]. Another study addressed these barriers in lack of access to the public toilet (inadequate shelves or countertops in placing supplies in preparation of CIC), difficult position to insert the catheter, lack of proper training and lack of community support and structural pathway trouble shooting in case of problems [9]. Another study showed that discontinuation of CIC tends to be personal variables (pain, resistant behavior of the child, difficulty in organizing the daily routine, UTI and lack of motivation) rather than demographic and medical characteristics, and significant predictors for non-used CIC were temporary discontinuation of the procedure, daily frequency of CIC and technical difficulties [18].
In this study the association of compliance before the education program, in a three-month follow-up and post education is significant (P Value 0.000), Faure, et al., cited by Rim, et al., reported that contacting the patient and requesting him/her to visit the clinic at a regular interval were very important in increasing adherence [16].
Regarding VUR, in this study, seven (29%) patients identified have VUR pre intervention, after 6 months of practicing the CIC The repeated MCUG showed the following: in pre -program three patients have bilateral VUR. One of them has reflux grade 5 in the left ureter and reflux grade 3 in other ureter, in post program there was bilateral reflux grade 5 which means an increase in one site, and the remaining have bilateral reflux grade 5. In post one of them has no VUR and the other has no reflux in one ureter while the reflux in the other ureter decreases from grade 5 to 3. Four of the patients have unilateral VUR, grade 2, 3, 4, 5, and two of them (grade 2 and 3) have no VUR in post program and in the third and 4th, the VUR remains static. In overall one patient out of seven (14.3%) the VUR increased in post program and 3 (42.9%) showed improvement in VUR. And in two of them (28.6%) VUR remained static. This result is similar to the study done after the introduction of CIC on Western Sweden for 89 patients who began CIC between the years 1977- 1985. It showed that the patients with isolated reflux or isolated dilatation complete normalization occurred in 5 of 11 and 12 of 16 patients respectively. Patients with combined dilatation and reflux were halve of children, the situation remained the same or even deteriorated so those with combined dilatation and reflux need more frequent follow-up with uro-radiology and assuring that CIC is carried out on a regular basis [19].
Equations [20]: n = (N/1+(N*E2 )
Where; n = sample size, N= population number, E = error (0,05), n= 40/1+(40*0.052) and n = 36
Conclusion
This study showed that despite the small sample size of the participants, CIC has a significant effect on improvement of renal abnormality (VUR), and it did not lead to an increase in frequency of UTI. Additionally, the education program showed a significant effect on compliance of the mothers of spina bifida children.
References
- Emmanuel A Ameh, Stephen W Bickler, Kokila Lakhoo, Benedict C Nwomeh DP. Paeds Surgery Part 1. 1st ed. Ameh. E A, Biickler. S W, Lakhoo. k, Nwomeh.B .C PoenaruD, editor. Paediatric Surgery: A Comprehensive Text book Volume 2. Seatle. WA. USA: Global HELP Organization; 2011. pp. 385-
- Liptak GS, El Samra A (2010) Optimizing health care for children with spina bifida. Dev Disabil Res Rev 16(1): 66-75.
- (2013) National Institute Of Neurological Disorders And Stroke. Spina Bifida Fact Sheet | National Institute of Neurological Disorders and Stroke 13-309.
- Rabiu TB, Adeleye AO (2013) Prevention of myelomeningocele: African perspectives. Child’s Nervous System 29(9): 1533-1540.
- Eltahir A Elsheikh G, Ibrahim SA (2009) Neural Tube defects in Omdurman Maternity Hospital, Sudan. Khartoum Medical Journal 2(2).
- Omer IM, Abdullah OM, Mohammed IN, Abbasher LA (2016) Research: Prevalence of neural tube defects Khartoum, Sudan August 2014-July 2015. BMC Res Notes 9: 1-4.
- Ambartsumyan L, Rodriguez L (2018) Bowel management in children with spina bifida. J Pediatr Rehabil Med 11(4): 293-301.
- Dik P, Klijn AJ, van Gool JD, de Jong-de Vos van Steenwijk CCE, de Jong TPVM (2006) Early Start to Therapy Preserves Kidney Function in Spina Bifida Patients. Eur Urol 49(5): 908-913.
- Seth JH, Haslam C, Panicker JN (2014) Ensuring patient adherence to clean intermittent self-catheterization. Patient Prefer Adherence 8: 191-198.
- Oakeshott P, Hunt GM (1992) Intermittent self catheterization for patients with urinary incontinence or difficulty emptying the bladder. British Journal of General Practice 42(359): 253-255.
- Segal ES, Deatrick JA, Hagelgans NA (1995) The determinants of successful self-catheterization programs in children with myelomeningoceles. J Pediatr Nurs 10(2): 82-88.
- Girotti ME, MacCornick S, Perissé H, Batezini NS, Almeida FG (2011) Determining the variables associated to clean intermittent selfcatheterization adherence rate: One-year follow-up study. International Braz J Urol 37(6): 766-772.
- Newman DK, Willson MM (2011) Review of intermittent catheterization and current best practices. Urol Nurs 31(1): 12-28.
- Neel KF, Salem MA, Soliman SM, Al-Hazmi H, Gomha AB, et al. (2008) Acceptance and compliance of clean intermittent catherization among Saudi patients. Saudi Med J 29(7): 1014-1017.
- Afsar SI, Yemisci OU, Cosar SNS, Cetin N (2013) Compliance with clean intermittent catheterization in spinal cord injury patients: A long-term follow-up study. Spinal Cord 51(8): 645-649.
- Lee SR, Lee IS, Oh SJ, Kim SH, Chin YR (2018) Adherence to the clean intermittent catheterization following a customized intensive education program for patients with emptying failure. Journal of Korean Academy of Community Health Nursing 29(4): 467-475.
- Mathew G (2006) Study to assess compliance and selected factors affecting compliance to clean intermittent catheterization (CIC) in childern with spina bifida. RGUHS.
- Faleiros F, Pelosi G, Warschausky S, Tate D, Käppler C, et al. (2018) Factors influencing the use of intermittent bladder catheterization by individuals with spina Bifida in Brazil and Germany. Rehabilitation Nursing 43(1):4 6-51.
- Lindehall B, Claesson I, Hialmas K, Jodal U (1991) Effect of Clean intermittent catheterisation on radiological appearance of the upper urinary Tract in children with myelomeningocele. Br J Urol 67(4): 415-419.
- Naing NN (2003) Determination of sample size. Malays J Med Sci 10(2): 84-86.






 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.